Persistent COVID-19: Stunning Two-Year Infection Sparks Urgent Alarm
A man had COVID-19 for more than two years without ever clearing the virus, a case that has captured the attention of researchers worldwide due to its unprecedented duration and implications. This rare and concerning situation involved a 41-year-old immunocompromised man in the US who harbored an active SARS-CoV-2 infection for over 750 days— far beyond the typical course of the disease. Unlike cases of long COVID, where symptoms persist but the virus is no longer actively replicating, this patient’s body never cleared the virus. Instead, the virus persisted and continually mutated inside his system, offering scientists a unique window into viral evolution and the risks posed by prolonged infections.
Understanding Persistent COVID-19 Infections in Immunocompromised Individuals
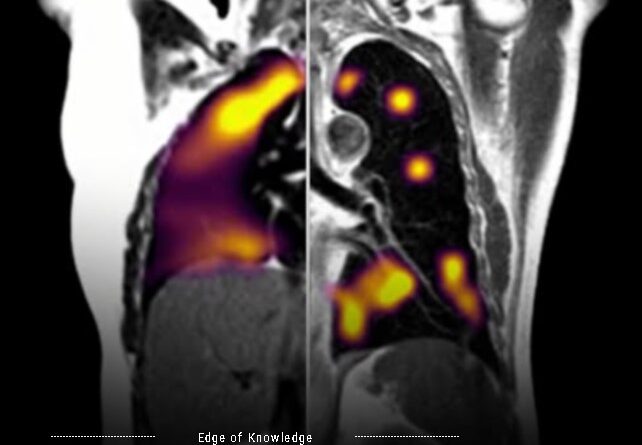
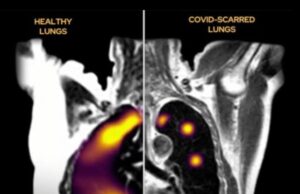
Persistent infections are most commonly seen in patients with significantly weakened immune systems. In this case, the patient’s advanced HIV infection left him with a critically low T-cell count—only 35 cells per microliter, compared to the healthy range of 500 to 1,500. T-cells are vital immune defenders that help to identify and eliminate viral pathogens. Without sufficient T-cell activity, the body struggles to eradicate viruses, leading to chronic infections.
Between 2020 and 2022, this man was hospitalized five times with ongoing respiratory issues, headaches, and weakness. These symptoms reflected active viral replication rather than merely post-viral effects. Due to limited access to antiretroviral therapy during the early stages of his COVID-19 infection, his immune system remained compromised, allowing the virus to persist for more than two years.
How the Virus Evolved Over 750 Days of Infection
What makes this case particularly compelling is the way scientists tracked the evolution of the virus inside the patient. Through genetic analysis of multiple samples collected over time, researchers observed the virus accumulating mutations at a rate comparable to what is normally seen across entire populations during regular spread.
Among these mutations were several changes similar to those found in the Omicron variant, including alterations to the spike protein—the component SARS-CoV-2 uses to bind and enter human cells. This demonstrates that prolonged infection in an immunocompromised individual can create a kind of “miniature incubator,” where the virus can explore genetic changes that might confer advantages like increased transmissibility or immune evasion.
The Broader Implications for Public Health and Variant Emergence
This case highlights an important, though underappreciated, pathway for the emergence of new viral variants. While most variants arise from widespread community transmission, persistent infections in vulnerable hosts can serve as reservoirs for accelerated mutation. The concern is that such mutations might eventually allow the virus to bypass immunity or improve its fitness to spread more efficiently.
Fortunately, the mutated virus in this case did not become highly transmissible, but experts warn that this is not guaranteed in other cases. The risks are particularly high for populations with limited access to treatment and care, such as those with unmanaged HIV or other immunosuppressive conditions.
Why Addressing Persistent COVID-19 Is a Public Health Priority
Clearing persistent infections like the one seen in this patient is critical not only for the individual’s health but also for preventing the development of new, potentially dangerous variants. Accessible healthcare, including antiretroviral therapy for people with HIV, early access to COVID-19 antivirals, and comprehensive vaccination programs, are essential components in controlling persistent infections.
Regular monitoring of viral evolution in immunocompromised patients can also help identify concerning mutations early, potentially guiding public health responses before variants become widespread. This approach requires integrated healthcare systems with strong surveillance capacities and supportive care for vulnerable individuals.
Conclusion
The case of a man carrying an active COVID-19 infection for over two years underscores crucial lessons about viral persistence, mutation, and the dynamics of variant emergence. It emphasizes the interconnectedness of individual patient health and global public health outcomes. Targeted treatment, vigilant surveillance, and equitable healthcare access are key strategies in preventing the virus from gaining new footholds in vulnerable populations.
For those interested in the scientific details, the study titled “Characterisation of a persistent SARS-CoV-2 infection lasting more than 750 days in a person living with HIV: a genomic analysis” was published in The Lancet in September 2025 and offers an in-depth look at this unprecedented case.
This remarkable story reminds us that while the majority of COVID-19 cases resolve within weeks, the battles faced by immunocompromised individuals can be protracted and complex—calling for compassion, science-driven care, and unwavering public health commitment.